
A hiatal hernia occurs when a portion of the stomach, most often the upper part, bulges through an opening in the diaphragm. When this happens, it is common to experience acid reflux—the backflow of stomach acid into the esophagus. This condition can progress to gastroesophageal reflux disease (or GERD), which we explore in further detail below.
While someone with a small hiatal hernia may not have acid reflux or GERD, those with larger hiatal hernias often contend with uncomfortable and painful symptoms ranging from heartburn and regurgitation of food to chest pain and more.
At EmergeOrtho—Triangle Region, we have an entire team of board-certified, highly skilled physicians and surgeons who diagnose and treat hiatal hernias. Keep reading to learn more about the symptoms, causes, and treatment of hiatal hernias and how our general surgeons can help provide you with relief.
What Are the Symptoms of a Hiatal Hernia?
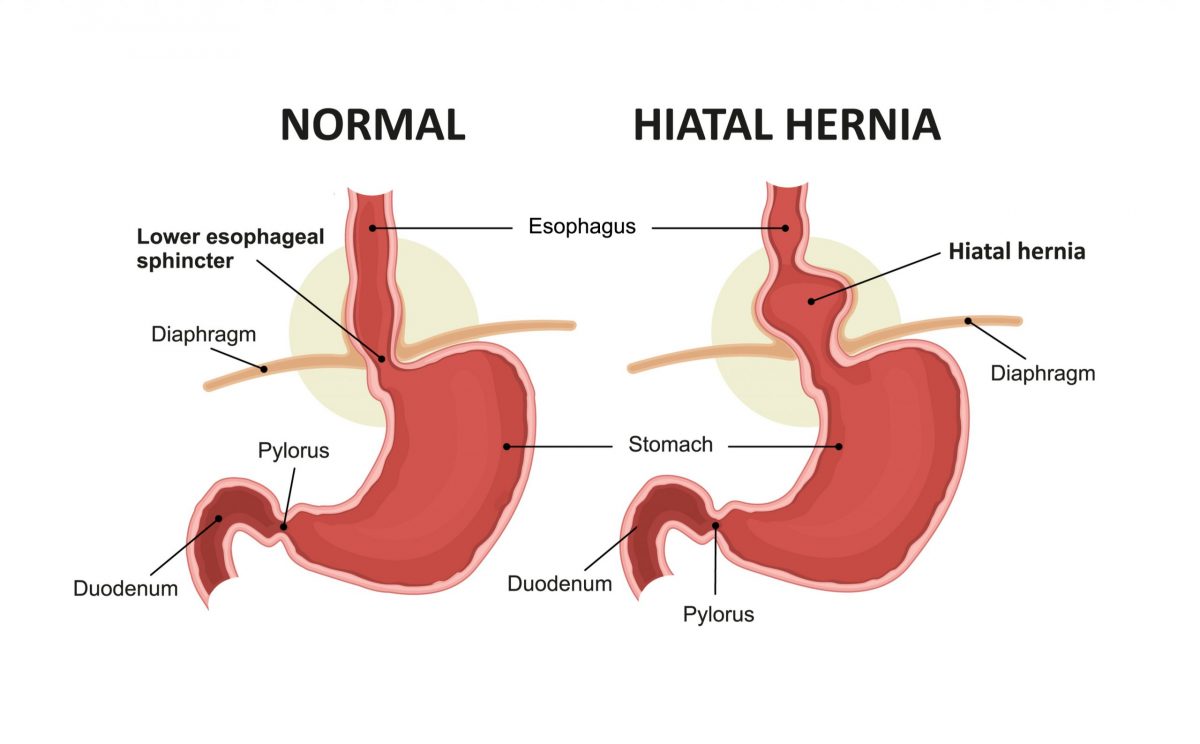
As put by our very own fellowship-trained surgeon Dr. Thomas Scarritt, a hernia is “Simply a hole.” For hiatal hernias, that hole is one that already exists in the diaphragm (allowing the esophagus to pass through). Over time, however, that space can enlarge and allow abdominal contents to bulge upwards into the chest. This hole becomes larger (often from the aging process and passage of time), resulting in increased abdominal pressure, leading to the weakening of the tough muscle layers.
Specific factors that can contribute to a hiatal hernia include:
- Obesity
- Pregnancy
- Constipation
- Chronic obstructive pulmonary disease (COPD)
- Trauma
- Previous surgeries
- Genetics
Symptoms of hiatal hernia can include:
- Heartburn
- Acid reflux
- Problems swallowing
- Pain in the chest and/or abdomen
- Shortness of breath
- Feeling full soon after eating
- Blood in your vomit
- Passing black stools (this can indicate gastrointestinal bleeding)
Can My Hernia Be Causing My Reflux?
Yes! As we mentioned earlier, it is common for people with hiatal hernia to have acid reflux, or gastroesophageal reflux (GER.) When GER progresses into GERD, a person may have a more severe form of reflux, with increased frequency of symptoms such as heartburn and regurgitation of food (often multiple times a week.) Individuals with GERD may also experience:
- Coughing
- Problems swallowing
- Wheezing when breathing
- Chest pain
Often, GERD symptoms become exacerbated when a person is lying down to sleep at night.
Although common, not everyone who has a hiatal hernia has GERD—and not everyone diagnosed with GERD has a hiatal hernia. The relationship between these conditions, however, makes it important to seek guidance from a physician specializing in hernias and GERD for a proper assessment.
How is a Hiatal Hernia Diagnosed?
There are several tests your physician may conduct to help determine the presence of a hiatal hernia as well as GERD:
- Upper GI swallow study. Patients drink “contrast” liquid before taking X-rays, enabling the physician to view the outline of the esophagus, stomach, and upper intestine.
- Upper endoscopy. A thin, flexible tube with a tiny light and camera (endoscope) is inserted into the throat to examine the esophagus and stomach.
- Esophageal manometry. This diagnostic test measures the rhythmic muscle contractions in your esophagus when you swallow. The doctor slides a probe into the esophagus and has the patient drink a glass of water.
How is Hiatal Hernia Treated By a Physician?
Hiatal hernia treatment depends on a patient’s specific diagnosis. For individuals with a small hiatal hernia who do not exhibit symptoms of acid reflux or GERD, a “watch-and-wait” approach may be all that is necessary. For someone with a hiatal hernia and GERD, however, surgery is likely needed. This is especially true if acid-reducing medications and other conservative treatments have failed to relieve symptoms.
Types of surgical procedures to repair a hiatal hernia (as well as GERD) include:
Fundoplication. Part of the excess stomach is wrapped around the esophagus (360 degrees) to form a valve that helps prevent contents of the stomach from going back up into the esophagus.
Toupet fundoplication. Rather than 360 degrees, the surgeon wraps the stomach closer to 270 degrees around the esophagus.
These procedures are typically laparoscopic and only require small incisions.
It is normal to experience soreness for the first two weeks or so following hiatal hernia surgery. And, as part of your recovery, your surgeon will prescribe a liquid diet, followed by pureed, soft, and—eventually—solid foods (typically staggered two-months.)
Many people successfully heal from hiatal hernia repair without the need for revision or further treatment measures.
To learn more about hiatal hernias, acid reflux, and GERD, watch this in-depth video interview with Dr. Scarritt. And, you can self-schedule your appointment with an EmergeOrtho—Triangle Region physician any time. Or, call us any time at (919) 281-1723.







